EMMA Endometrial Microbiome Metagenomic Analysis
The most comprehensive and precise panel, encompassing the most frequently detected and clinically relevant bacteria to evaluate the endometrium at the microbiological level
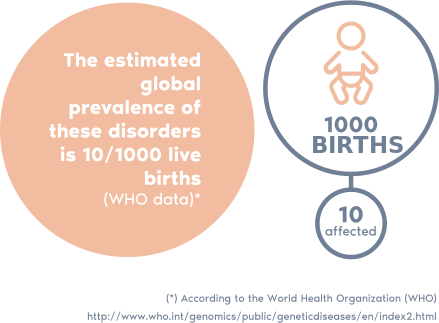
30% of infertile women
have pathogenic bacteria detected in their endometrium

Upgraded EMMA panel: the most precise panel available, developed after analysing over 70,000 clinical samples during the last 5 years
The upgraded EMMA panel now identifies bacteria at the species level, enabling more precise and targeted treatments
What is the EMMA test?
> EMMA is a test that analyses the endometrial microbiome to help identify abnormalities associated with a poor reproductive prognosis.
> EMMA assesses the endometrial microbiome, providing information about the most common and relevant bacteria, including those linked to higher pregnancy rates. EMMA also includes ALICE, which detects pathogenic bacteria that can cause chronic endometritis.
> Igenomix has analysed over 70,000 clinical samples during the last 5 years.
> Through our experience with the EMMA&ALICE tests, we have identified the bacterial pathogens most frequently detected in the endometrium.
> Based on this data, we have developed the most comprehensive and precise panel, encompassing all clinically relevant bacteria, with most identified at the species level, enabling a more precise and targeted treatments.
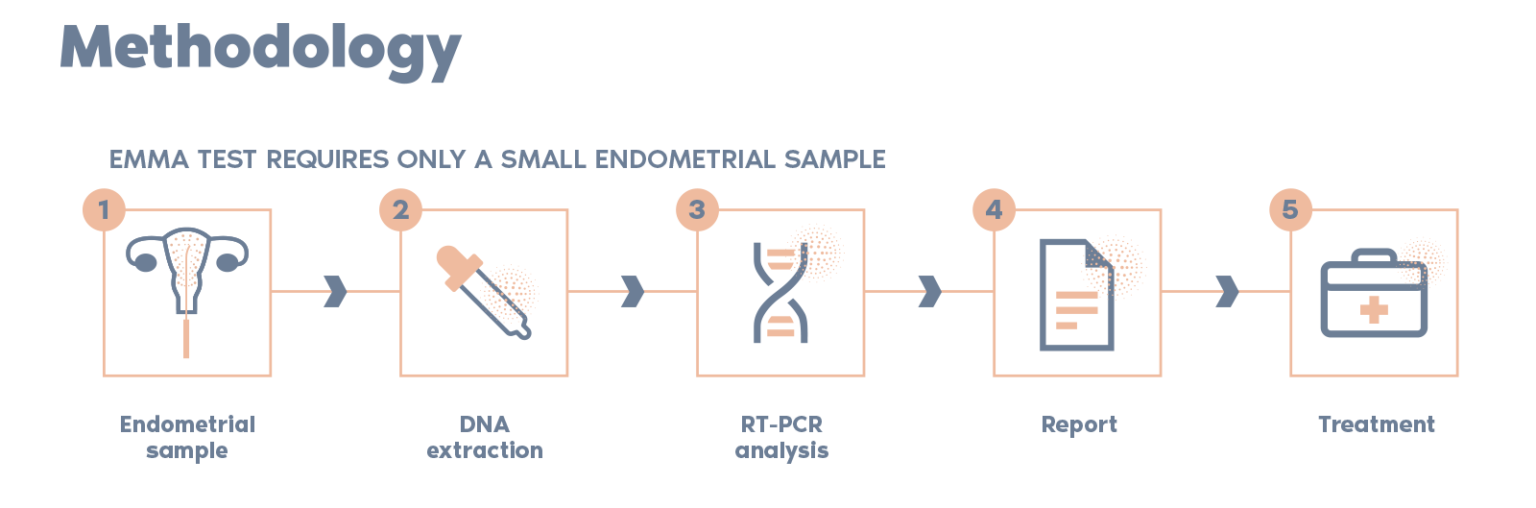
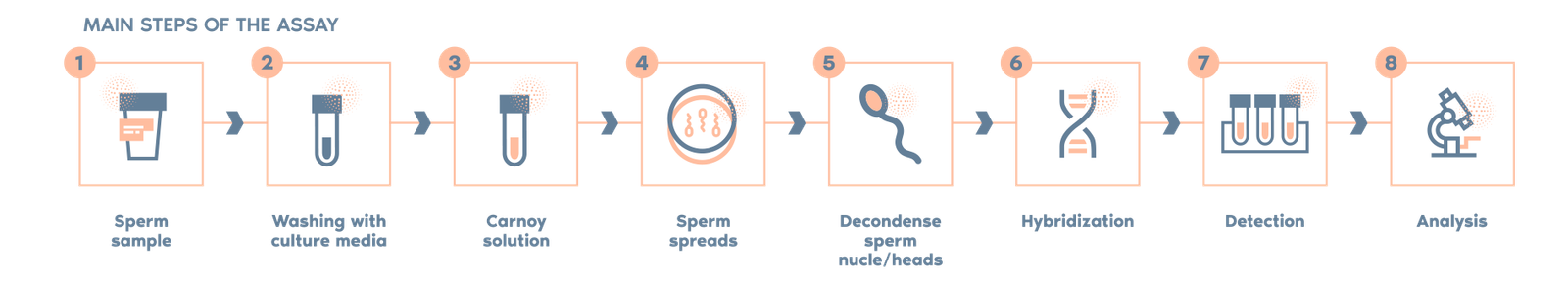
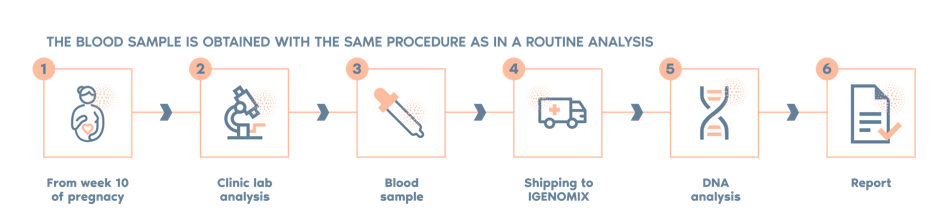
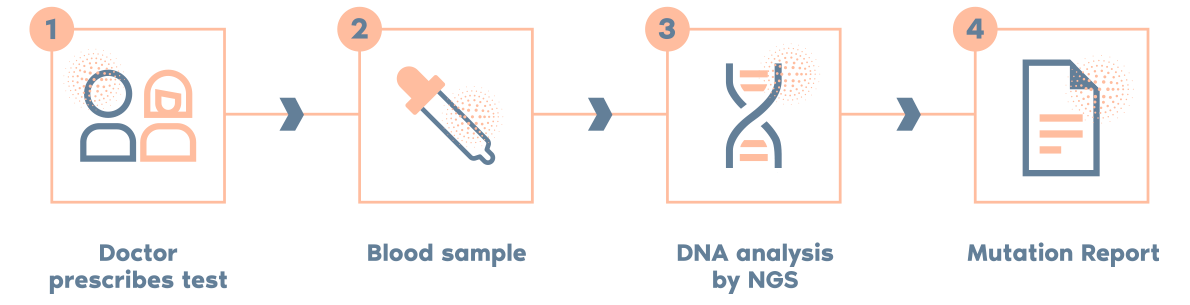
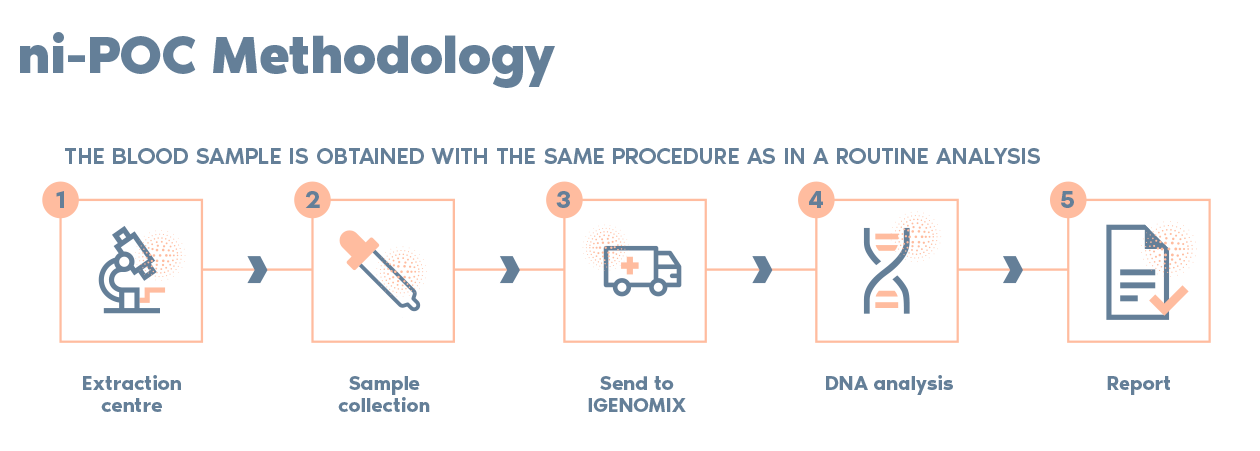
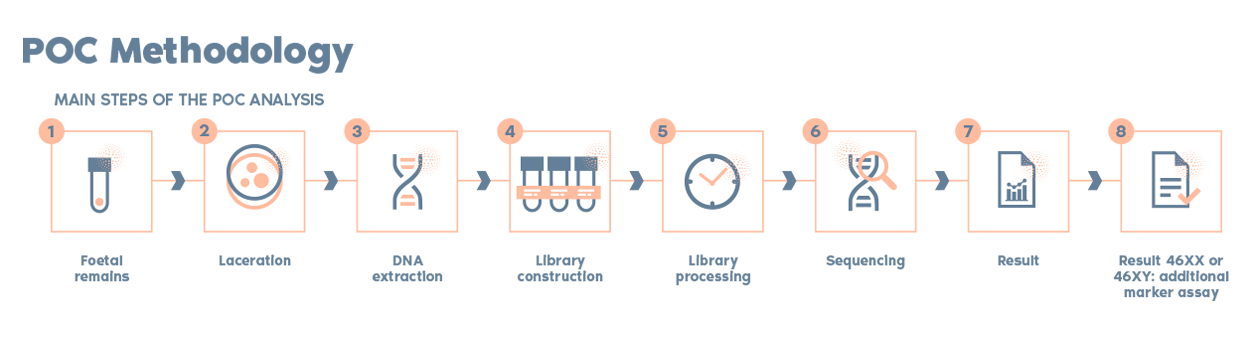
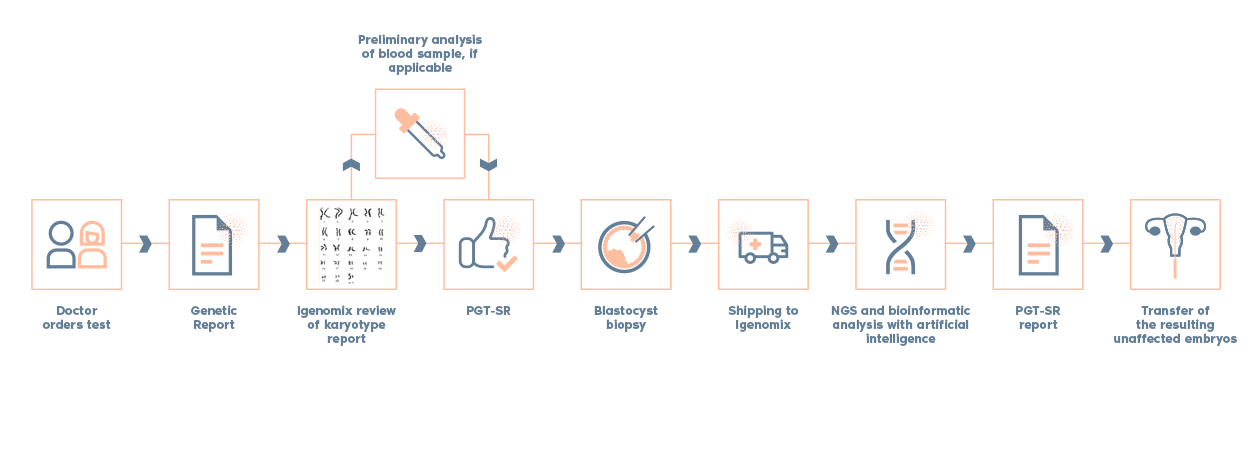
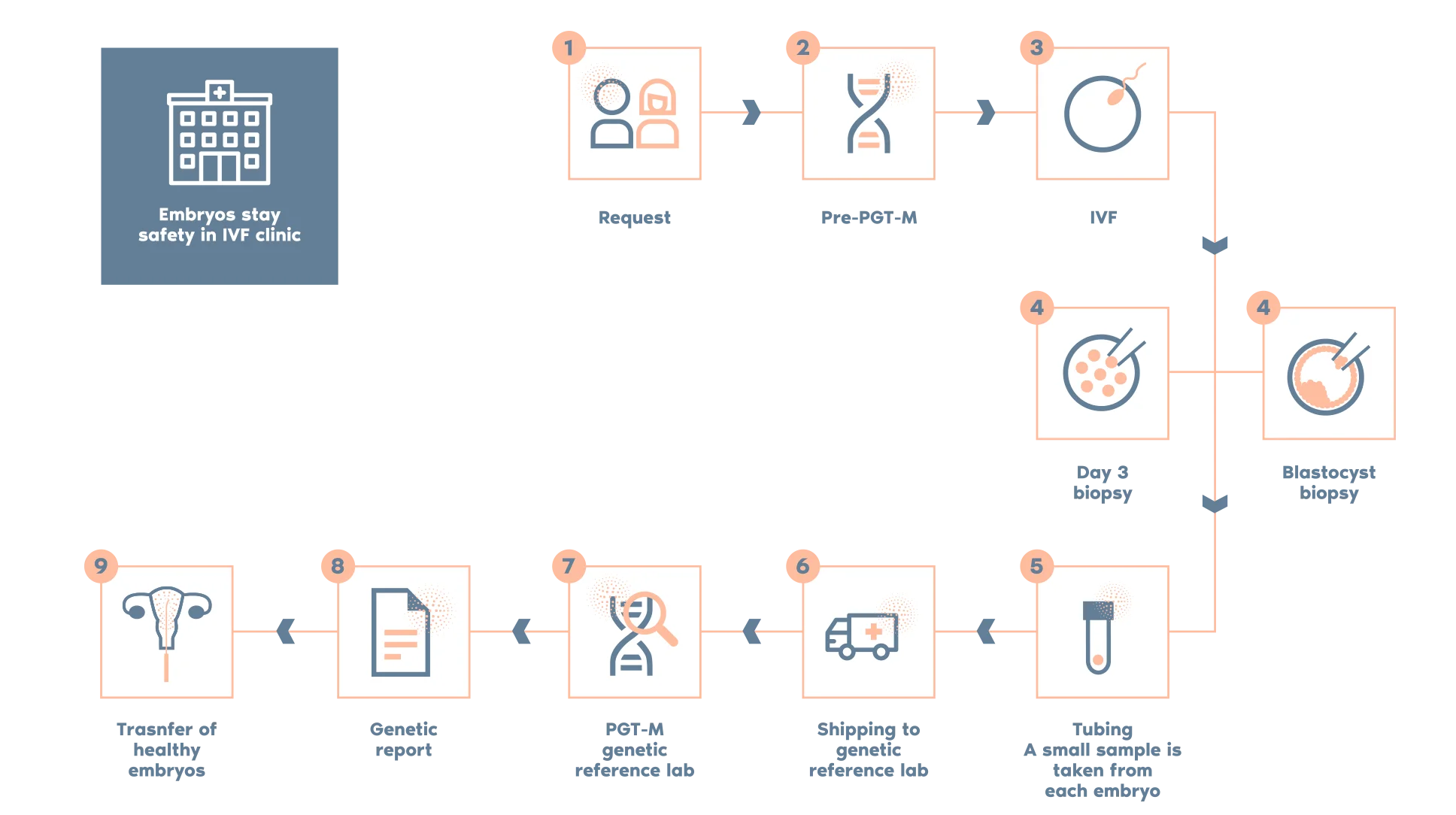
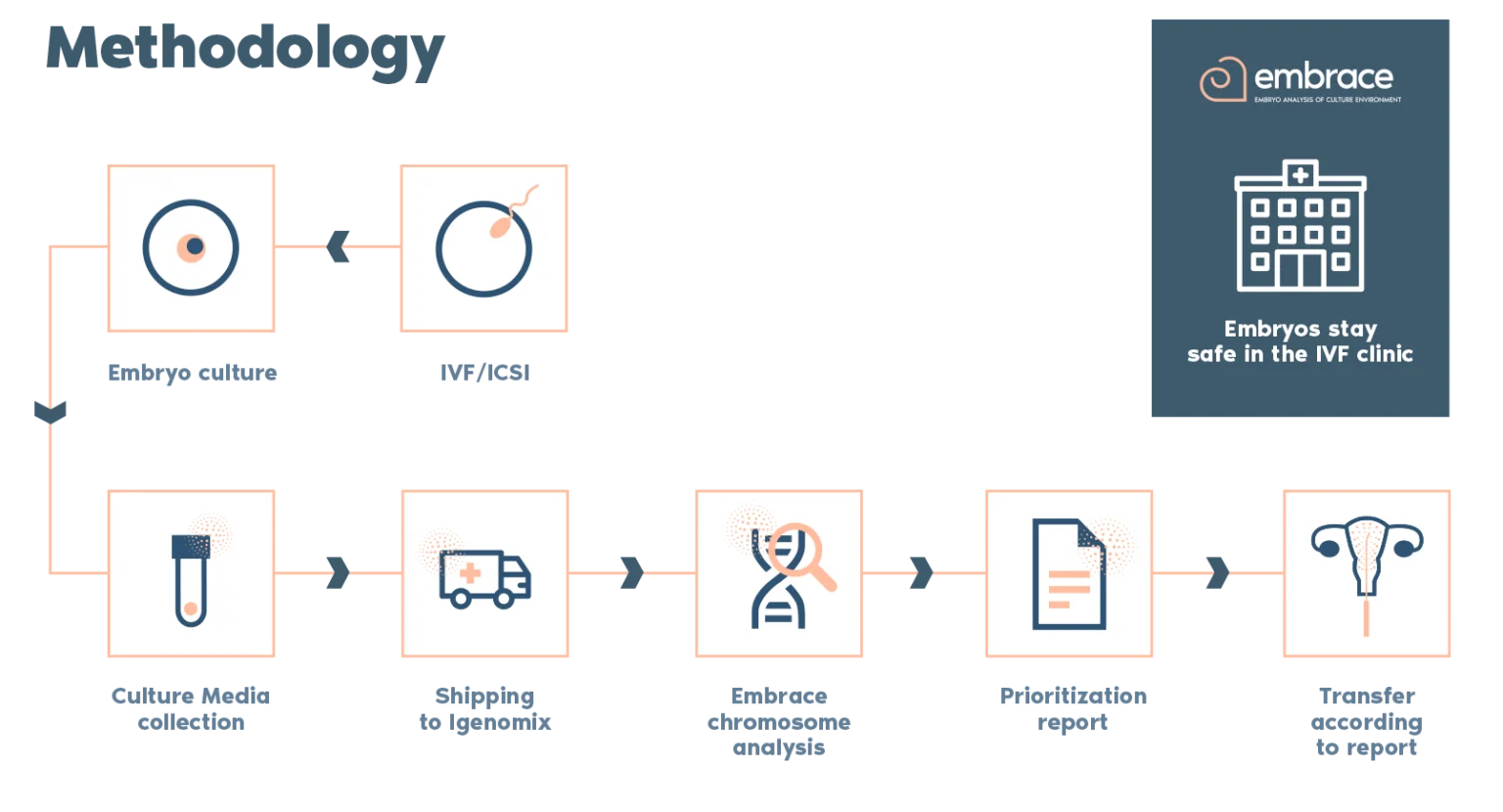
What is the procedure?
Why use EMMA test?
> EMMA uses the latest RT-PCR technology to provide endometrial microbiome information by analysing the presence and quantity of the most common and relevant bacterial pathogens of the reproductive tract.
> EMMA can determine the percentage of Lactobacillus present in the endometrium; low proportions of Lactobacillus are associated with poor reproductive outcomes
> EMMA also includes ALICE, which detects pathogenic bacteria that can cause chronic endometritis.
> EMMA determines whether the endometrial microbial environment is optimal or not for embryo implantation.
> If the endometrial microbial environment is not optimal for embryo implantation, a recommendation for a precise and targeted treatment is provided.
Who should use the EMMA?
> Patients with repeated implantation failure (RIF)
> Patients with repeated pregnancy loss (RPL)
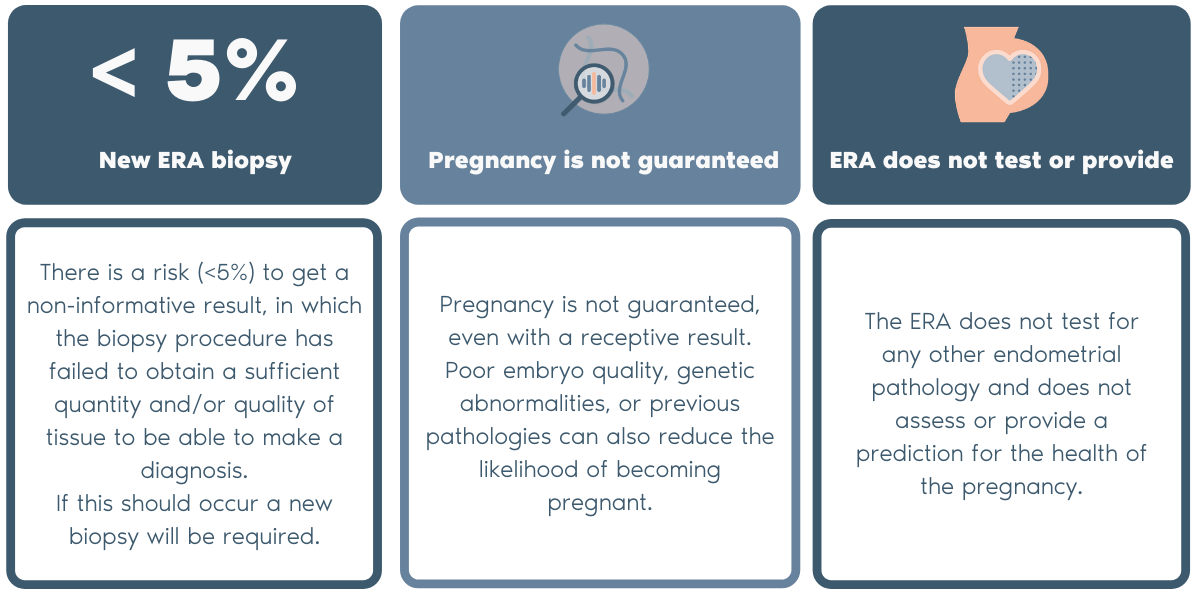
Test limitations
> These tests are not able to detect resistance to antibiotics
> A negative result doesn’t rule out the presence of other endometrial pathogens